Eisai’s lecanemab shows positive cognitive effects in Alzheimer’s disease.
Dear Readers
You will find attached results presented yesterday on lecanemab Clarity AS study at the Clinical Trials on Alzheimer’s disease (CTAD) conference in San Francisco. Eisai, BioArtic and Biogen have confirmed that the Phase III lecanemab data look strong on efficacy (27% on decline) and safety on Amyloid -related imaging abnormalities (ARIA) a major concern we had mentioned previously.
“During the study period, deaths occurred in 0.7% and 0.8% of participants in the lecanemab and placebo groups, respectively and no deaths were related to lecanemab or occurred with amyloid-related imaging abnormalities (ARIA) in the 18-month double- blind study period” says the Press Release attached.
One analyst came away from the presentation saying that major risks for a rapid U.S. FDA approval have been removed.
Have a nice read
…………………………………………………………………
Jean-Claude Muller Ph.D.
Executive Editor
![]()
phone: 33 6 76 84 71 60
mail: jcm9144@gmail.com
…………………………………………………………………

1.50 AM CET / 30-Nov-2022 / BioArctic (STO:BIOA B)
BioArctic’s partner Eisai presents results of lecanemab Phase 3 confirmatory Clarity AD study for Early Alzheimer’s disease at CTAD conference
Stockholm, November 30, 2022 – BioArctic AB’s (publ) (Nasdaq Stockholm: BIOA B) partner Eisai announced today that the results from the large global Phase 3 confirmatory Clarity AD clinical study of lecanemab (development code: BAN2401), an investigational anti-amyloid beta (Aβ) protofibril antibody for the treatment of mild cognitive impairment (MCI) due to Alzheimer’s disease (AD) and mild AD (collectively known as early AD) with confirmed presence of amyloid pathology in the brain, were presented at the 2022 Clinical Trials on Alzheimer’s Disease (CTAD) conference, in San Francisco, California and virtually.
Summary of presentations in the scientific session featuring lecanemab at CTAD
Design of Clarity AD study
Clarity AD was a global confirmatory Phase 3 placebo-controlled, double-blind, parallel-group, randomized study in 1,795 people with early AD (lecanemab group: 898, placebo group: 897) at 235 sites in North America, Europe, and Asia. The participants were randomized 1:1 to receive either placebo or lecanemab 10 mg/kg IV biweekly, and the randomization was stratified according to clinical subgroups (MCI due to AD or mild AD), presence or absence of concomitant approved AD symptomatic medication at baseline (e.g., acetylcholinesterase inhibitors, memantine, or both), ApoE4 status and geographical region. Eligibility criteria allowed patients with a broad range of comorbidities/comedications, including but not limited to hypertension, diabetes, heart disease, obesity, renal disease and anti-coagulants. As a result of Eisai’s recruitment strategy of diversity in the Clarity AD study, 4.5% and 22.5% of the randomized participants in the U.S. were Black and Hispanic, respectively.
The primary endpoint was change from baseline at 18 months in the CDR-SB[1] (Clinical Dementia Rating Sum of Boxes), the global cognitive and functional scale, and key secondary endpoints were the change from baseline at 18 months in amyloid Positron Emission Tomography (PET) using Centiloids, AD Assessment Scale – Cognitive Subscale 14 (ADAS-Cog14[2]), AD Composite Score (ADCOMS[3]) and AD Cooperative Study-Activities of Daily Living scale for mild cognitive impairment (ADCS MCI-ADL[4]). In addition, longitudinal changes in brain tau pathology as measured by tau PET (n=257), and cerebrospinal fluid (CSF) biomarkers of AD pathology (n=281) were evaluated in optional sub-studies.
Efficacy results of Clarity AD
Mean change of CDR-SB from baseline at 18 months as the primary endpoint was 1.21 and 1.66 for lecanemab and placebo groups, respectively. Lecanemab treatment resulted in highly statistically significant results, reducing clinical decline on the global cognitive and functional scale, compared with placebo at 18 months by -0.45 (95% Confidence Interval (CI): -0.67, -0.23; P=0.00005), representing a 27% slowing of decline. Starting as early as six months (difference: -0.17 [95% CI: -0.29, -0.05]; P<0.01), and increasing in absolute difference over time across all time points every 3 months, the treatment showed highly statistically significant changes in CDR-SB from baseline compared to placebo (all p-values are less than 0.01) (Figure 1).
All key secondary endpoints also showed highly statistically significant results compared with placebo (P<0.001). In the amyloid PET sub-study, treatment with lecanemab showed statistically significant reduction in amyloid plaque burden at all timepoints starting at 3 months. Mean change in Centiloids at 18 months was -55.5 and 3.6 for lecanemab and placebo groups, respectively (mean difference: -59.1 [95% CI: -62.6, -55.6]; P<0.00001). Lecanemab slowed decline of cognitive function by 26% on ADAS-Cog14 at 18 months (mean difference: -1.44 [95% CI: -2.27, -0.61]; P=0.00065). In the ADCOMS assessment, lecanemab slowed disease progression by 24% at 18 months (mean difference: -0.050 [95% CI: -0.074, -0.027]; P=0.00002). Lecanemab slowed decline of activities of daily living by 37% on ADCS MCI-ADL at 18 months (mean difference: 2.016 [95% CI: 1.208, 2.823]; P<0.00001). In addition, the primary stratified analysis showed consistent results in CDR-SB, ADAS-Cog14 and ADCS MCI-ADL at 18 months of treatment with lecanemab in all subgroups of disease stage (MCI due to AD or mild AD), ApoE4 status (non-carriers, carriers), presence or absence of concomitant approved AD symptomatic medication, and region (North America, Asia, Europe).
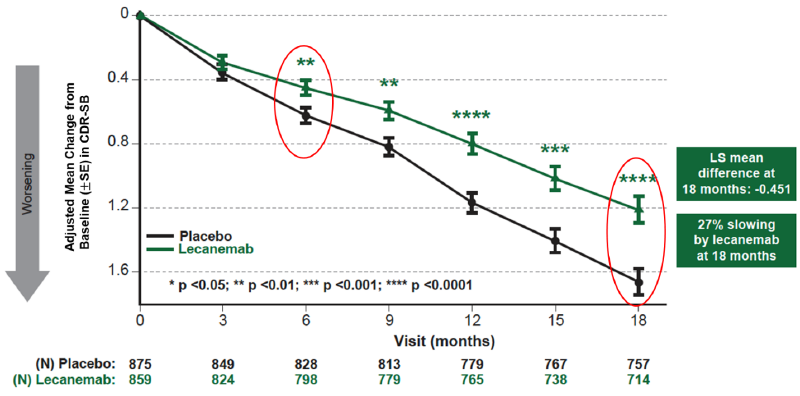
Figure1. CDR-SB as Primary endpoint change (18 months)
Safety Results of Clarity AD
The most common adverse events (>10%) in the lecanemab group were infusion reactions (lecanemab: 26.4%; placebo: 7.4%), ARIA-H (combined cerebral microhemorrhages, cerebral macrohemorrhages, and superficial siderosis; lecanemab: 17.3%; placebo: 9.0%), ARIA-E (edema/effusion; lecanemab: 12.6%; placebo: 1.7%), headache (lecanemab: 11.1%; placebo: 8.1%), and fall (lecanemab: 10.4%; placebo: 9.6%). Infusion reactions were largely mild-to-moderate (grade 1-2: 96%) and occurred on the first dose (75%).
During the study period, deaths occurred in 0.7% and 0.8% of participants in the lecanemab and placebo groups, respectively and no deaths were related to lecanemab or occurred with amyloid-related imaging abnormalities (ARIA) in the 18-month double- blind study period. Serious adverse events were experienced by 14.0% of participants in the lecanemab group and 11.3% of participants in the placebo group. Treatment-emergent adverse events occurred in 88.9% and 81.9% of participants in the lecanemab and placebo groups, respectively. Treatment-emergent adverse events leading to drug withdrawal occurred in 6.9% and 2.9% of participants in the lecanemab and placebo groups, respectively.
Overall, lecanemab’s ARIA incidence profile was within expectations based on the Phase 2b trial results. ARIA-E events were largely mild-to-moderate radiographically (91% of those who had ARIA-E), asymptomatic (78% of those who had ARIA-E), occurred within the first 3 months of treatment (71% of those who had ARIA-E) and resolved within 4 months of detection (81% of those who had ARIA-E). Among the 2.8% of lecanemab-treated subjects with symptomatic ARIA-E, the most commonly reported symptoms were headache, visual disturbance, and confusion. The incidence of symptomatic ARIA-H was 0.7% in the lecanemab group and 0.2% in the placebo group. No imbalance was observed in isolated ARIA-H (i.e., ARIA-H in participants who did not also experience ARIA-E) between lecanemab (8.9%) and placebo (7.8%). ARIA-E and ARIA-H were less common in ApoE4 non-carriers versus carriers, with higher frequency in ApoE4 homozygous carriers vs ApoE4 heterozygous carriers. In the core study and subsequent open-label extension study, rates of deaths with concurrent cerebral macrohemorrhage were 0.1% in both the placebo group (1/897) and the lecanemab group (2/1608). The two cases on lecanemab occurred in the open-label extension study. Both cases had significant comorbidities and risk factors including anticoagulation contributing to macrohemorrhage or death. Therefore, it is Eisai’s assessment that the deaths cannot be attributed to lecanemab.
Imaging, plasma, and CSF biomarkers assessments of Clarity AD
Biomarkers assessments on amyloid, tau and neurodegeneration with lecanemab administration were conducted using imaging, plasma and CSF. Amyloid biomarkers showed early and sustained amyloid reversal effects in CSF and plasma Aβ 42/40 ratio with lecanemab treatment. Mean amyloid PET was 22.99 Centiloids at 18 months of lecanemab treatment which was below threshold for amyloid positivity of 30 Centiloids. Tau biomarkers showed that removing amyloid improved CSF and plasma p-tau (p-tau181), downstream of amyloid in the AD pathology pathway. Tau PET analysis showed that lecanemab treatment slowed tau accumulation in the temporal lobe as well as improved total tau (t-tau) compared to placebo. As for biomarkers of neurodegeneration, lecanemab improved glial fibrillary acidic protein (GFAP) in plasma, a marker of astrocyte activation, and neurogranin in CSF, a marker of synaptic dysfunction, improved to normal levels by treatment, while there was no significant difference in neurofilament light chains in CSF or plasma between lecanemab and placebo.
Clarity AD results in context
AD is a progressive neurological disorder that severely impacts people living with the condition and their loved ones. With the increased global aging population, AD has become a critical issue for society and healthcare systems. New therapeutic agents that act on the disease pathology are needed. The treatment goals for early AD are to have sustained effects on cognitive functions, activities of daily living and psychiatric symptoms, to maintain independence longer by slowing progress of the disease and to improve or maintain quality of life.
In the confirmatory Clarity AD study, lecanemab demonstrated consistency of results across scales of cognition and function and subgroups (race, ethnicity, comorbidities). Lecanemab treatment showed 31% lower risk of converting to next stage of disease by Global CDR assessment (Hazard Ratio: 0.69). A slope analysis using CDR-SB based on observed data and extrapolation to 30 months showed that lecanemab takes 25.5 months to reach same level as placebo at 18 months, indicating a 7.5 month slowing of progression. Modeling simulations based on the Phase 2b trial data suggest that lecanemab may slow the rate of disease progression by 2.5-3.1 years and has the potential to help people remain in the earlier stages of AD for a longer period of time. In addition, it was shown to maintain the health-related quality of life and reduce the burden on caregivers (23-56% reduction in score worsening). The convergence of evidence across cognition and function, disease progression, health-related quality of life, and caregiver burden demonstrate that lecanemab treatment may provide meaningful benefits to patients, their care partners, physicians, and society.
Eisai serves as the lead of lecanemab development and regulatory submissions globally. They are hosting a live webcast of the scientific session featuring the lecanemab presentations, which can be viewed live on the investors section of the Eisai Co., Ltd. website. The content will be available on demand afterward.
—
This release discusses investigational uses of an agent in development and is not intended to convey conclusions about efficacy or safety. There is no guarantee that such an investigational agent will successfully gain health authority approval.
This information is information that BioArctic AB (publ) is obliged to disclose pursuant to the EU Market Abuse Regulation. The information was released for public disclosure, through the agency of the contact persons below, on November 30, 2022, at 01:50 a.m. CET.
For further information, please contact:
Gunilla Osswald, CEO
E-mail: gunilla.osswald@bioarctic.se
Phone: +46 8 695 69 30
Oskar Bosson, VP Communications and IR
E-mail: oskar.bosson@bioarctic.se
Phone: +46 70 410 71 80
About Clarity AD
|
Study title |
A Study to Confirm Safety and Efficacy of Lecanemab in Participants With Early Alzheimer's Disease (Clarity AD) |
|
Study population |
1,795 participants with mild cognitive impairment (MCI) due to Alzheimer’s disease (AD) and mild AD (collectively known as early AD) with confirmed presence of amyloid pathology in the brain in the global study, and an additional 111 subjects ongoing in China. |
|
Treatment administered |
10 mg/kg bi-weekly of lecanemab or placebo |
|
Duration of treatment |
18 months |
|
Study locations |
Japan, the U.S., Europe, China, South Korea, Canada, Australia, Singapore |
|
Primary endpoint |
Change from baseline in the Clinical Dementia Rating-Sum of Boxes (CDR-SB) at 18 months |
|
Key secondary endpoints |
Change From Baseline at 18 months in: |
|
Analysis Object |
An efficacy analysis was conducted in a modified intention-to-treat population of 1,734 subjects (859 lecanemab group and 875 placebo group). The safety analysis was performed on all 1,795 randomized participants (lecanemab group: 898, placebo group: 897). |
About lecanemab (BAN2401)
Lecanemab is an investigational humanized monoclonal antibody for Alzheimer's disease (AD) that is the result of a strategic research alliance between BioArctic and Eisai. Lecanemab selectively binds to neutralize and eliminate soluble toxic Aβ aggregates (protofibrils) that are thought to contribute to the neurodegenerative process in AD. As such, lecanemab may have the potential to have an effect on disease pathology and to slow down the progression of the disease. Currently, lecanemab is being developed as the only late-stage anti-Aβ antibody that can be used for the treatment of early AD without the need for titration, enabling full treatment effect from day one.
The Clarity AD open-label extension is underway with treatment initiated after completion of the Core period to further evaluate the safety and efficacy of lecanemab. In addition, the lecanemab Phase 3 clinical study AHEAD 3-45 is ongoing for individuals with preclinical (asymptomatic) AD, meaning they are clinically normal and have intermediate or elevated levels of brain amyloid. AHEAD 3-45 is conducted as a public-private partnership between the Alzheimer’s Clinical Trial Consortium, funded by the National Institute on Aging, part of the National Institutes of Health, and Eisai. In 2021, lecanemab was selected for the Tau NexGen clinical study for Dominantly Inherited Alzheimer’s disease (DIAD), as a background anti-amyloid treatment when exploring combination therapies with anti-tau treatments. The study, which is ongoing, is conducted by Dominantly Inherited Alzheimer Network Trials Unit (DIAN-TU), led by Washington University School of Medicine in St. Louis. Furthermore, Eisai has performed a lecanemab subcutaneous dosing Phase 1 study and the subcutaneous formulation is currently being evaluated in the Clarity AD open label extension study.
In July 2022, the U.S. Food and Drug Administration (FDA) accepted Eisai’s Biologics License Application (BLA) for lecanemab under the Accelerated Approval Pathway and granted Priority Review. The Prescription Drug User Fee Act action date (PDUFA) is set for January 6, 2023. The FDA has agreed that the results of Clarity AD can serve as the confirmatory study to verify the clinical benefit of lecanemab. In an effort to secure traditional FDA approval for lecanemab as soon as possible, Eisai submitted the BLA through the FDA’s Accelerated Approval Pathway so that the agency could complete its review of all lecanemab data with the exception of the data from the confirmatory Clarity AD study. In March 2022, Eisai began submitting application data, with the exception of Clarity AD data, to Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) under the prior assessment consultation system. Eisai will discuss the results of Clarity AD study with regulatory authorities in the U.S., Japan and Europe with the aim to file for traditional approval in the U.S., and to submit marketing authorization applications in Japan and Europe by the end of the first quarter 2023.
About the collaboration between BioArctic and Eisai
Since 2005, BioArctic has a long-term collaboration with Eisai regarding the development and commercialization of drugs for the treatment of Alzheimer’s disease. The most important agreements are the Development and Commercialization Agreement for the lecanemab antibody, which was signed in December 2007, and the Development and Commercialization agreement for the antibody BAN2401 back-up for Alzheimer’s disease, which was signed in May 2015. In March 2014, Eisai and Biogen entered into a joint development and commercialization agreement for lecanemab. Eisai is responsible for the clinical development, application for market approval and commercialization of the products for Alzheimer’s disease. BioArctic has right to commercialize lecanemab in the Nordic under certain conditions and is currently preparing for commercialization in the Nordics together with Eisai. BioArctic has no development costs for lecanemab in Alzheimer’s disease and is entitled to payments in connection with regulatory filings, approvals, and sales milestones as well as royalties on global sales.
About BioArctic AB
BioArctic AB (publ) is a Swedish research-based biopharma company focusing on disease-modifying treatments for neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease and ALS. BioArctic focuses on innovative treatments in areas with high unmet medical needs. The company was founded in 2003 based on innovative research from Uppsala University, Sweden. Collaborations with universities are of great importance to the company together with its strategically important global partner Eisai in Alzheimer disease. The project portfolio is a combination of fully funded projects run in partnership with global pharmaceutical companies and innovative in-house projects with significant market and out-licensing potential. BioArctic’s Class B share is listed on Nasdaq Stockholm Mid Cap (ticker: BIOA B). For more information about BioArctic, please visit www.bioarctic.com.
[1] CDR-SB is a numeric scale used to quantify the various severity of symptoms of dementia. Based on interviews of people living with AD and family/caregivers, qualified healthcare professionals assess cognitive and functional performance in six areas: memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care. The total score of the six areas is the score of CDR-SB, and CDR-SB is also used as an appropriate item for evaluating the effectiveness of therapeutic drugs targeting the early stages of AD.
[2] ADAS-cog is the most common cognitive assessment instrument used in AD clinical trials all over the world. ADAS-cog14 consists of 14 competencies: word recall, commands, constructional praxis, object and finger naming, ideational praxis, orientation, word recognition, remembering word recognition instructions, comprehension of spoken language, word finding difficulty, spoken language ability, delayed word recall, number cancellation, and maze task. ADAS-cog has been used in clinical trials for earlier stages of AD including MCI.
[3] Developed by Eisai, combines items from the ADAS-cog scale for assessing cognitive functions, MMSE and the CDR scale for evaluating the severity of dementia to enable highly sensitive detection of changes in clinical functions of early AD symptoms and changes in memory
[4] ADCS MCI-ADL assesses the competence of patients with MCI in activities of daily living (ADLs), based on 24 questions to the patient’s partner about actual recent activities of daily living.
Last News
- Pétrole et semi-conducteurs : Une histoire qui se répète mais qui ne se ressemble pas.
- Oil and semiconductors: a story that repeats itself but is not the same.
- Stroke : An update
Events
News archives
- March 2024
- February 2024
- January 2024
- November 2023
- September 2023
- July 2023
- April 2023
- March 2023
- January 2023
- December 2022
- November 2022
- October 2022
- August 2022
- June 2022
- May 2022
- April 2022
- March 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- October 2018
- June 2018
- May 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- September 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- June 2014
- May 2014
- April 2014
- March 2014
- January 2014
- November 2013
- September 2013
- July 2013
- May 2013
- April 2013
- March 2013
- January 2013
- December 2012
- November 2012
- October 2012
- March 2012





